Asepsis

Asepsis is the state of being free from disease-causing micro-organisms (such as pathogenic bacteria, viruses, pathogenic fungi, and parasites).[1] There are two categories of asepsis: medical and surgical.[1] The modern day notion of asepsis is derived from the older antiseptic techniques, a shift initiated by different individuals in the 19th century who introduced practices such as the sterilizing of surgical tools and the wearing of surgical gloves during operations.[2] The goal of asepsis is to eliminate infection, not to achieve sterility.[1] Ideally, a surgical field is sterile, meaning it is free of all biological contaminants (e.g. fungi, bacteria, viruses), not just those that can cause disease, putrefaction, or fermentation.[1] Even in an aseptic state, a condition of sterile inflammation may develop. The term often refers to those practices used to promote or induce asepsis in an operative field of surgery or medicine to prevent infection.[3]
History
[edit]The modern concept of asepsis evolved in the 19th century through multiple individuals. Ignaz Semmelweis showed that hand washing prior to delivery reduced puerperal fever. Despite this, many hospitals continued to practice surgery in unsanitary conditions, with some surgeons taking pride in their bloodstained operating gowns.[4] It was not until after reading of the findings by Louis Pasteur that Joseph Lister introduced the use of carbolic acid as an antiseptic, and in doing so, reduced surgical infection rates.[5] Lawson Tait shifted the movement then from antisepsis to asepsis, instilling practices such as a strict no-talking policy within his operating room and drastically limiting the number of people to come in contact with a patient's wound.[6] Ernst von Bergmann also introduced the autoclave, a device used for the practice of the sterilization of surgical instruments.[7]

But, everything from operating room uniforms to gloves was pioneered by William Halsted. Preceding modern-day scrubs attire, Halsted implemented a no street clothes policy in his operating room, opting to wear a completely white, sterile uniform consisting of a duck suit, tennis shoes, and skullcap.[2] This helped to prevent the introduction of infections into open wounds.[2] Additionally, Halsted would sterilize the operation site with alcohol, iodine and other disinfectants and use drapes to cover all areas except for the site.[2] In his department at Johns Hopkins Hospital, he enforced an extreme hand washing ritual consisting of soaking in harmfully strong chemicals like permanganate and mercury bichloride solution as well as scrubbing with stiff brushes.[2] The damage to a surgical nurse's hands compelled him to create the earliest form of the surgical gloves with the Goodyear Rubber Company.[2] These gloves became a part of the aseptic surgery standard when Dr. Joseph Colt Bloodgood and several others began wearing them for that particular purpose.[8]
Antisepsis vs. Asepsis
[edit]The line between antisepsis and asepsis is interpreted differently, depending on context and time.[5] In the past, antiseptic operations occurred in people's homes or in operating theaters before a large crowd.[5] Procedures for implementing antisepsis varied among physicians and experienced constant changes.[5] Until the late 19th century, physicians rejected the connection between Louis Pasteur's germ theory that bacteria caused diseases and antiseptic techniques.[9] At the end of the 19th century, Joseph Lister and his followers expanded the term "antisepsis" and coined "asepsis", with the justification that Lister had initially "suggested excluding septic agents from the wound from the start."[5] Generally, however, asepsis is seen as a continuation of antisepsis since many of the values are the same, such as a "germ-free environment around the wound or patient", and techniques pioneered under both names are used in conjunction today.[5]
Method
[edit]Asepsis refers to any procedure that is performed under sterile conditions. This includes medical and laboratory techniques (such as with bacterial cultures). There are two types of asepsis — medical and surgical.[1] Medical or clean asepsis reduces the number of organisms and prevents their spread; surgical or sterile asepsis includes procedures to eliminate micro-organisms from an area and is practiced by surgical technologists and nurses.[1] Ultimately, though, successful usage of aseptic operations depends on a combination of preparatory actions.[10] For example, sterile equipment and fluids are used during invasive medical and nursing procedures.[10] The largest manifestation of such aseptic techniques is in hospital operating theaters, where the aim is to keep patients free from hospital micro-organisms.[11]

While all members of the surgical team should demonstrate good aseptic technique, it is the role of the scrub nurse or surgical technologist to set up and maintain the sterile field.[12][13] To prevent cross-contamination of patients, instruments are sterilized through autoclaving or by using disposable equipment; suture material or xenografts also need to be sterilized beforehand.[14] Basic aseptic procedures includes hand washing, donning protective gloves, masks and gowns, and sterilizing equipment and linens.[11] Medical aseptic techniques also includes curbing the spread of infectious diseases through quarantine, specifically isolation procedures based on the mode of disease transmission.[11] Within contact, droplet and airborne isolation methods, two different procedures emerge: strict isolation vs. reverse isolation.[11] Strict isolation quarantines patients to prevent them from infecting others, while reverse isolation prevents vulnerable patients from becoming infected.[11]
Related infections
[edit]In aseptic conditions, a "chronic low-level inflammation" known as sterile inflammation may develop as a result of trauma, stress, or environmental factors.[15] As in infections caused by pathogens or microbes, the immune response is regulated by host receptors.[3] Tissue damage resulting from non-infectious means are caused by DAMPs molecules released after injury or cell death has occurred, which are able to stimulate inflammation response.[3] Diseases associated with sterile inflammation include Alzheimer's disease, atherosclerosis, as well as cancer tumor growth due to "immune cell infiltration."[3] Additionally, aseptic tissue damage may arise from corticosteroid injections, which are drugs used to treat musculoskeletal conditions such as carpal tunnel and osteoarthritis, though this tends to result from improper aseptic technique.[16][17]
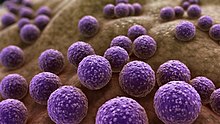
Despite efforts to preserve asepsis during surgery, there still persists a 1-3% chance of a surgical site infection (SSI).[18] Infections are categorized as superficial incisional, deep incisional, or organ; the first type are confined to the skin, the second to muscles and nearby tissues, and the third to organs not anatomically close to the operation site.[18][19] The exact modes of infection depend on the types of surgery, but the most common bacteria that are responsible for SSIs are Staphylococcus aureus, coagulase-negative staphylococci, Escherichia coli, and Enterococcus spp.[20] The CDC emphasizes the importance of both antiseptic and aseptic approaches in avoiding SSIs, especially since Staphylococcus aureus, among other bacteria, are able to evolve drug-resistant strains that can be difficult to treat.[21] In 2017, nearly 20,000 patients in the United States died from Staphylococcus aureus in comparison to the 16,350 from diagnosed HIV.[22][23]
See also
[edit]- Antiseptic
- Barrier nursing
- Body substance isolation
- Cleanliness
- Contamination control
- Disinfectant (measurements of effectiveness)
- Ignaz Semmelweis
- Sterilization (microbiology)
- Transmission-based precautions
References
[edit]- ^ a b c d e f Burke, Alene. "Standard Precautions, Transmission Based, Surgical Asepsis: NCLEX-RN || RegisteredNursing.org". www.registerednursing.org. Retrieved 2020-04-21.
- ^ a b c d e f Markel, Howard. An anatomy of addiction. New York: Pantheon Books.
- ^ a b c d Chen, Grace Y.; Nuñez, Gabriel (19 November 2010). "Sterile inflammation: sensing and reacting to damage". Nature Reviews. Immunology. 10 (12): 826–837. doi:10.1038/nri2873. ISSN 1474-1733. PMC 3114424. PMID 21088683.
- ^ Millard, Candice (2011). Destiny of the republic: a tale of madness, medicine and the murder of a president. New York: Doubleday. ISBN 978-0-385-52626-5. OCLC 700205578.
- ^ a b c d e f Schlich, Thomas (July 2012). "Asepsis and Bacteriology: A Realignment of Surgery and Laboratory Science1". Medical History. 56 (3): 308–334. doi:10.1017/mdh.2012.22. ISSN 0025-7273. PMC 3426977. PMID 23002302.
- ^ Flack, Harvey. Lawson Tait. Thomas Vicary Lecture.
- ^ "History of Infection Control and its Contributions to the". Medscape. Retrieved 2020-04-21.
- ^ "William Stewart Halsted". portraitcollection.jhmi.edu. Retrieved 2020-04-21.
- ^ "Developments in bacteriology - Attempts to prevent illness and disease – WJEC - GCSE History Revision - WJEC". BBC Bitesize. Retrieved 2020-04-21.
- ^ a b "Aseptic Surgery". research.uci.edu. Retrieved 2020-04-21.
- ^ a b c d e "Medical Asepsis (Clean Technique)" (PDF). Indiana Department of Health.
- ^ "Microbiology Techniques & Troubleshooting". Science Buddies.
- ^ "Bios 318 Microbiology methods manual". www.ruf.rice.edu.
- ^ Yool, Donald A. Small Animal Soft Tissue Surgery. CABI.
- ^ Feldman, Noa; Rotter-Maskowitz, Aviva; Okun, Eitan (2015-11-01). "DAMPs as mediators of sterile inflammation in aging-related pathologies". Ageing Research Reviews. Damage-associated molecular patterns and their pathological relevance in ageing. 24 (Pt A): 29–39. doi:10.1016/j.arr.2015.01.003. ISSN 1568-1637. PMID 25641058. S2CID 33283933.
- ^ "Injectable Corticosteroids". www.hopkinsmedicine.org. Retrieved 2020-04-21.
- ^ Holland, Christian; Jaeger, Lothar; Smentkowski, Ulrich; Weber, Beate; Otto, Christina (15 June 2012). "Septic and Aseptic Complications of Corticosteroid Injections". Deutsches Ärzteblatt International. 109 (24): 425–430. doi:10.3238/arztebl.2012.0425. ISSN 1866-0452. PMC 3394381. PMID 22787504.
- ^ a b "Surgical Site Infections". www.hopkinsmedicine.org. 22 November 2019. Retrieved 2020-04-21.
- ^ "Surgical Site Infections - Health Encyclopedia - University of Rochester Medical Center". www.urmc.rochester.edu. Retrieved 2020-04-21.
- ^ Owens, C. D.; Stoessel, K. (November 2008). "Surgical site infections: epidemiology, microbiology and prevention". The Journal of Hospital Infection. 70 (Suppl 2): 3–10. doi:10.1016/S0195-6701(08)60017-1. ISSN 0195-6701. PMID 19022115.
- ^ "Superbug, super-fast evolution". evolution.berkeley.edu. April 2008. Retrieved 2020-04-21.
- ^ Kourtis, Athena P. (2019). "Vital Signs: Epidemiology and Recent Trends in Methicillin-Resistant and in Methicillin-Susceptible Staphylococcus aureus Bloodstream Infections — United States". MMWR. Morbidity and Mortality Weekly Report. 68 (9): 214–219. doi:10.15585/mmwr.mm6809e1. ISSN 0149-2195. PMC 6421967. PMID 30845118.
- ^ "Basic Statistics | HIV Basics | HIV/AIDS | CDC". www.cdc.gov. 2020-03-20. Retrieved 2020-04-21.
